Victory Friday | Issue 115
Orthopedic Insights: Diaphragm, Quit Pulling My Leg (& Arm & Neck…) • Cable Shoulder In & Out • Trunk Rotation Check-In • Leg Length Double-Victory: Indications & Bonus Metrics to Nail LLD Diagnosis
“A fit body, a calm mind, a house full of love: these things cannot be bought; they must be earned.” ~ Naval Ravikant
Victory Friday is a weekly digest of reflections, insights, and tools from the world of functional manual and performance medicine. It is a free weekly publication. To support Victory Friday with a paid subscription, click below:
It’s a holiday Friday! The clinic may be closed this week but the lessons and insights continue to flow: the profound (and increasingly whole-body) connections to the diaphragm, a potent shoulder and rotational trunk stretch-strength strategy (and a test to see if you need it), and a double Victory from found leg length differentials: all little reminders capable of big changes! Enjoy!
What I’m Into: Diaphragm, Quit Pulling My Leg (and Arm and Neck…). I continue to find the root cause of many common, chronic problems “living” in the diaphragm.
For a few years I have seen a strong connection between diaphragm stiffness and pelvis (and hip) alignment and mobility deficits1.
This year, more than ever, I find the diaphragm is highly culpable for many upper body issues, namely:
• chronic neck pain and stiffness
• shoulder pain and stiffness
Struggling with a stubborn neck and/or shoulder problem? Check out the diaphragm!
Renegade Orthopedics is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Cool Exercises I Like. Cable Shoulder In & Out. Avid readers know I’m a big fan of exercises that:
• emphasize rotation and elongation
• combine mobility (loaded stretching) and strength
As I continue to look for tools to enhance whole-body fascial mobility, and functional multi-planar strength, I stumbled upon this gem. courtesy of strength coach Justin Lienhard:
It appears nameless, so I’m calling it a kneeling, Cable Shoulder In & Out. But it loads more than just the shoulder:
What I like about it:
• the loaded cable2 provides a deep fascial stretch along multiple fascial lines from the hand, through the scapula, into the ribcage, pelvis and even the leg.
• the active “in to out” pull-through motion strengthens into a reciprocal (gait- and athletic-specific) movement pattern.
• the horizontal force provides a rare strength input into the transverse plane: in my opinion the most important (and often most problematic) plane of movement in our body.
Joe’s Articles. Trunk Rotation Check-In. Want to check in with that rotational, transverse plane mobility?
This oldie, from iRunFar.com and a part of my mobility self-assessment series, assesses basic transverse plane motion of the spine and pelvis: Performance Mobility, Part 2: Trunk Rotation

And while the metric is also a restorative exercise, my preferred — and far more effective — way to improve ribcage rotation is by using a foam roller3, first.
Victory Friday. Leg Length Double-Victory: Indications & Bonus Metrics to Nail LLD Diagnosis. This past month saw two big victories over chronic hip and leg pain — all thanks to finding and addressing relevant leg length discrepancies (LLD).
A while back we first covered LLD’s: the challenges (and stigmas) to accurate diagnosis, treatment strategies, and long-term management4
We then outlined six metrics to determine a relevant LLD:
1. Pelvic height: Assess the pelvis in standing or functional movement for elevation on one side by checking the iliac crest, ASIS, and PSIS; all must be higher on one side to potentially indicate a leg length discrepancy (LLD), though height alone is insufficient.
2. Pelvic mobility: Confirm pelvic elevation through mobility testing of flexion and extension in each half-pelvis; symmetrical motion or bilateral restrictions with neutral alignment supports a static LLD, while asymmetrical restrictions may indicate pelvic rotation instead.
3. Ankle length & the Supine-to-Sit Test: Direct ankle length measurement in supine is unreliable due to positioning variability, but a consistent (no change in) leg length difference when moving from supine to long-sitting (removing pelvic motion) provides a positive, though incomplete, indicator for LLD.
4. Greater trochanter height: Standing assessment of greater trochanter height is a strong indicator of LLD, as few factors besides actual bony differences in the femur or lower leg affect it; four positive metrics up to this point suggest at least 90% accuracy for a static LLD.
And two functional tests:
5. Vertical Compression Test (VCT): This test applies vertical compression from the thorax downward; an inefficient response (bending or twisting) indicates discontinuity like LLD, and improved efficiency with a corrective lift under the short leg confirms the system prefers the correction.
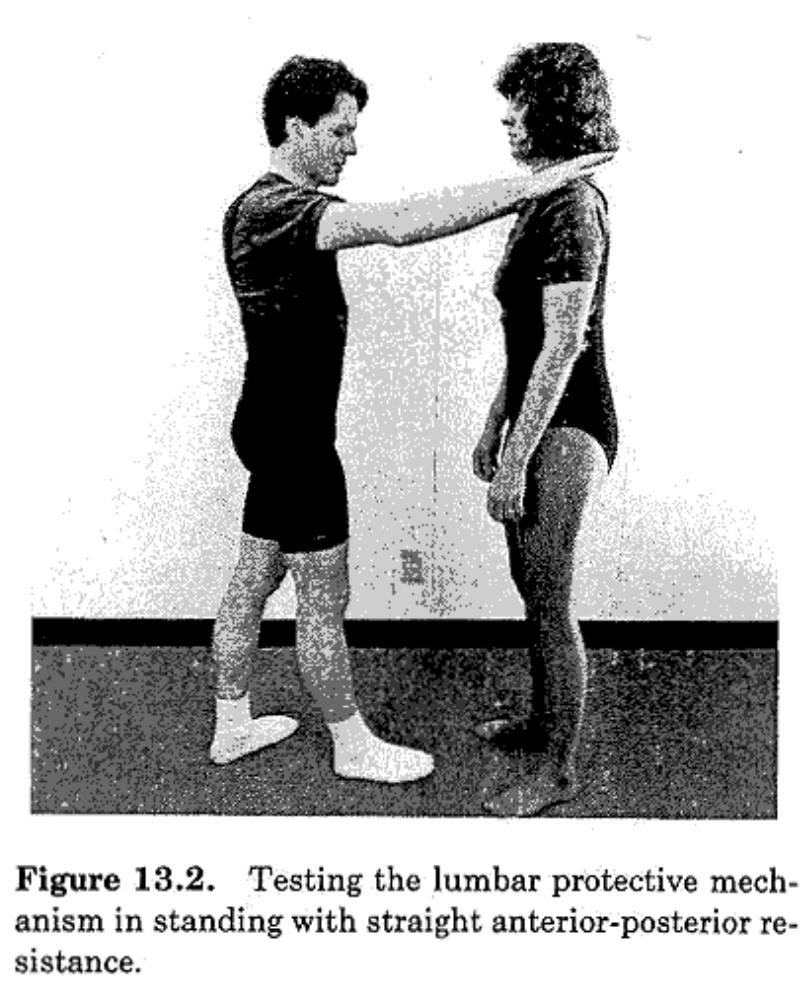
6. Lumbar Protective Mechanism (LPM): In a staggered stance, progressive force on the shoulders tests automatic anterior core stability; an inefficient response (using lumbar muscles or breaking posture) improves with a corrective under the short leg, showing the system prefers equalization for better core engagement
Generally:
A. Positive findings from at least three out of the first four measured metrics are a strong (90+%) positive for LLD.
B. A significant difference (both PT-measurable and patient-perceived) in function in at least one functional test is a strong positive for a corrective (height-increasing) insert in the shoe of the shorter leg.
This past month presented two cases:
• A 30-something ultramarathon runner with chronic hip pain, stiffness and weakness, with relatively new onset plantar foot pain.
• A 20-something former collegiate track runner who was limited by chronic hip pain his entire college career. And despite “retiring” — with no racing or intense training — his hip pain persists.
Both clients demonstrated:
• pelvic and hip alignment and mobility asymmetry
• thoracic cage mobility loss
Yet, after treating to restore thoracic spine, pelvis and hip mobility:
• hip pain did not improve, and
• motion and alignment gains made in the first visit, were lost upon re-examination at second visit
I seldom screen hard for leg length differential…until a comprehensive treatment approach I know to be successful fails to make any improvement. In such cases, I then look deeper.
Upon closer examination, both clients:
• tested 4/4 for the alignment, length, mobility and special test metrics
• tested objectively better for core stability (using LPM)
For treatment, both clients:
• received a 4-6mm full-length cork insert for trial use in all footwear for two weeks (to be used with all significant weightbearing)
And, I am happy to report that after two weeks:
Both clients report significant breakthroughs in pain relief, mobility, strength
and functional tolerance: they feel better running!
For me, in part this was simply another day at the office. Yet like many Victories, I share them not because they are profound, but because things such as LLDs are so often overlooked.
And, when addressed, the solution is so simple and easy!
However, this recent double Victory also generated further useful insight into LLDs, including helpful indications and a new, 7th test metric.
Leg Length Indications. How might we narrow our screening to target only those clients with a potential relevant LLD? Here are some indications:
• Repetitive Impact Athletes. Nearly all relevant (pain- and dysfunction-producing) leg length differentials occur in people who engage in impact athletics and/or accrue a lot of time-on-feet.
Runners are most common: three impacts per second over minutes and hours (or even days). But it could be any athlete5, especially if they also have a job or side-activity with a lot of time-on-feet.
• Treatment Recidivism. As I mentioned, a flag for me is when I perform thorough and comprehensive treatment to the spine, pelvis and hips, and both motion and alignment regress completely between visits. Client regression isn’t rare, but if you do robust hands-on work, they work hard on a home plan, and they are limited in activity…yet they come back at square one? A sinister input is at play.
• Relentless Pain. Multi-dimensional treatment — mobility, strength, efficiency optimization, and rest — fails to get any pain relief. And they feel pain across many different activities: not just running or sports, but walking, standing and sometimes even sitting and lying down.
• “Just Enough But Not Too Much”. In over a decade of refined testing and treatment, I find most highly athletic people with relevant LLDs have a difference of 4-8 millimeters.
Why? Because a difference smaller than that is “absorbable”: the body is able to compensate and “absorb” the difference without significant dysfunction.
And a difference larger than 8mm? These folks have far less tolerance to any significant athletic activity and are never active enough to make it into your office. People with a 10mm LLD simply don’t become runners because it immediately feels terrible when they run.
Bonus Metric! Based on these recent cases I have developed a 7th objective test for LLD determination:
7. Restorative treatment to the system makes the leg length difference worse
(The Decompensation Rule).
When working with an athlete with a suspected LLD, you might find a 4-5mm difference in supine at the ankle6, and a similar difference at the greater trochanter in standing.
But nearly always, the ribcage and pelvis will show motion loss and asymmetry.
And when you restore motion and correct for symmetry…the leg length difference will get worse.
Why?
Because restorative treatment removes the positive compensation!
How this becomes a robust LLD test:
If a clinician:
• finds a leg length difference, and
• finds a pelvic and ribcage asymmetry, and
• treats the system to restore motion
and the leg length difference improves? That indicates the leg length difference was functional — or created by pelvic and thoracic spine bends, twists and rotations — and not a bony difference!
But if the LLD gets worse, congratulations: you have successfully stripped away the body’s compensatory effort to absorb the difference.
The analog nature of this is potent; it is now a crucial element in both my diagnosis and treatment process for a LLD.
It’s win-win: either I treat the system and the LLD is even “more real” and actionable (w/shoe inserts for the short side), or it improves. Either way, we are a step closer to dysfunction resolution.
Take-Aways. Screen for Leg Length Discrepancies for Every Stubborn Lower Quarter Case (Using the 7 Tests)! If you or your clients show indications — namely stubborn pain, motion loss and alignment imbalances, and they are an impact athlete — thoroughly test for LLD using this system.
“Sell” the client on an insert using the functional tests — can they feel improved function with a correction? — then perform at least a two-week trial insert7 in the short leg shoe.
If correct and necessary, then symptom, mobility, alignment and even strength improvements are right around the corner! Good luck!
Issue 115 is complete!
Help people move, function and feel better: please share this publication!
Thanks for reading, and have a great weekend,
Issue 40. Diaphragm Dysfunctions Hindering Hips. Diaphragm (and thoracic cage) mobility loss can restrict hip and pelvic mobility and alignment. Two cases presented with restricted hips, pelvic rotations or torsions, and failed to maintain mobility or neutral alignment despite direct treatments. Comprehensive three-dimensional diaphragm treatment freed and/or unlocked pelvic and hip mobility. The diaphragm’s fascial connections profoundly affect hip function beyond breathing and core stability, so thoracic mobility and diaphragm assessment are essential for lower quarter clients.
Cable: consistent tension regardless of position within the movement.
Issue 58: (Lateral) Ribcage Foam-Rolling. Outlines the use of sustained foam roll pressure for diaphragm and lower thoracic spinal mobilization, including two published columns:
• lateral and posterior diaphragm
• anterior diaphragm (vertical and horizontal)
Issue 52: “Leveling Success” & Joe’s Six Metrics for Leg Length Discrepancy. A balanced approach to diagnosing and treating clinically relevant leg length discrepancies (LLD) avoids extremes of over-prescribing corrections or dismissing them entirely. Thorough assessment clusters multiple data points for high diagnostic accuracy, with full-length shoe inserts recently resolving chronic pain and restoring symmetry in two runners.
The six metrics are: Pelvic height, Pelvic mobility, Ankle length & the Supine-to-Sit Test, Greater trochanter height, Vertical Compression Test, Lumbar Protective Mechanism.
Functional testing demonstrates benefits to patients, inexpensive materials like cork sheets are recommended, and regular re-assessment is essential.
Conversely: athletes with shorter durations on feet, without impact, and with a lot of variety — weightlifters, pickleball players — may be less likely to present with a stubborn injury driven by a LLD — especially if they have a sitting job or are a student.
unchanged by the Supine-Sit test
I always prefer full-length to a heel lift, to avoid any angular changes to the foot and ankle.




