Victory Friday | Issue 87
Orthopedic Insights: If you're >40, It Might Not Be Achilles • Plumbing & Electric Nerve Treatment • Side Door Hip Mobility • 3 Stride Strategies for Achilles • Inflating “Deflated” Lower Legs
"The opposite of faith isn’t doubt, it is certainty." ~ Anne Lamott
Victory Friday is a weekly digest of reflections, insights, and tools from the world of functional manual and performance medicine. It is a free weekly publication. To support Victory Friday with a paid subscription, see below.
It’s Friday again! It’s funny how life self-assembles. The rules (or curses?) of threes. And while it may be superstition, it is human nature to recognize patterns.
I saw a couple this week, related to lower leg preservation.
What I’m Into:
“Most Massage Therapists Treat People Like Pieces of…Paper”. A refrain repeated several times this week.
I’ve been treated by scores of massage therapists. Not a single one did any other treatment position than supine (front side) and prone (back) — unless I asked for (or insisted upon) it.
Work one side. Flip over. Work the other.
We’re three-dimensional beings with fascial tissues that spiral in all directions. Medial and lateral tissues in sidelying are crucial!
To learn more about how medial and lateral tissue unlock forward (and backward) motion, see Joe’s Articles.
“If You’re Over 40, It Might Not (Actually) Be Your Calf or Achilles”. Calf and Achilles-area pain is scourge of older runners.
Once they get it, so it seems, it can last a stubbornly — if not a suspiciously — long time.
Damaged tissue heals. Mild sprains take 1-3 weeks. Moderate strains, 6-12 weeks. Full ruptures and repairs? 6-12 months.
So how, then, do many runners suffer from calf and Achilles pain for months or years?
Here’s how:
They (unknowingly) continue to stress it. (See Joe’s Articles and this week’s Victory)
Or:
It’s not actually the calf (muscle) or Achilles (tendon).
For clients (runners or otherwise) with chronic lower leg, calf and Achilles pain — especially cases that take more than a few weeks of standard treatment (rest, stretch, strength), something else is aggravated, causing pain.
That something else? Nerves, usually.
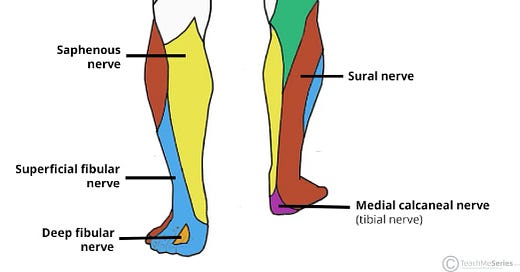
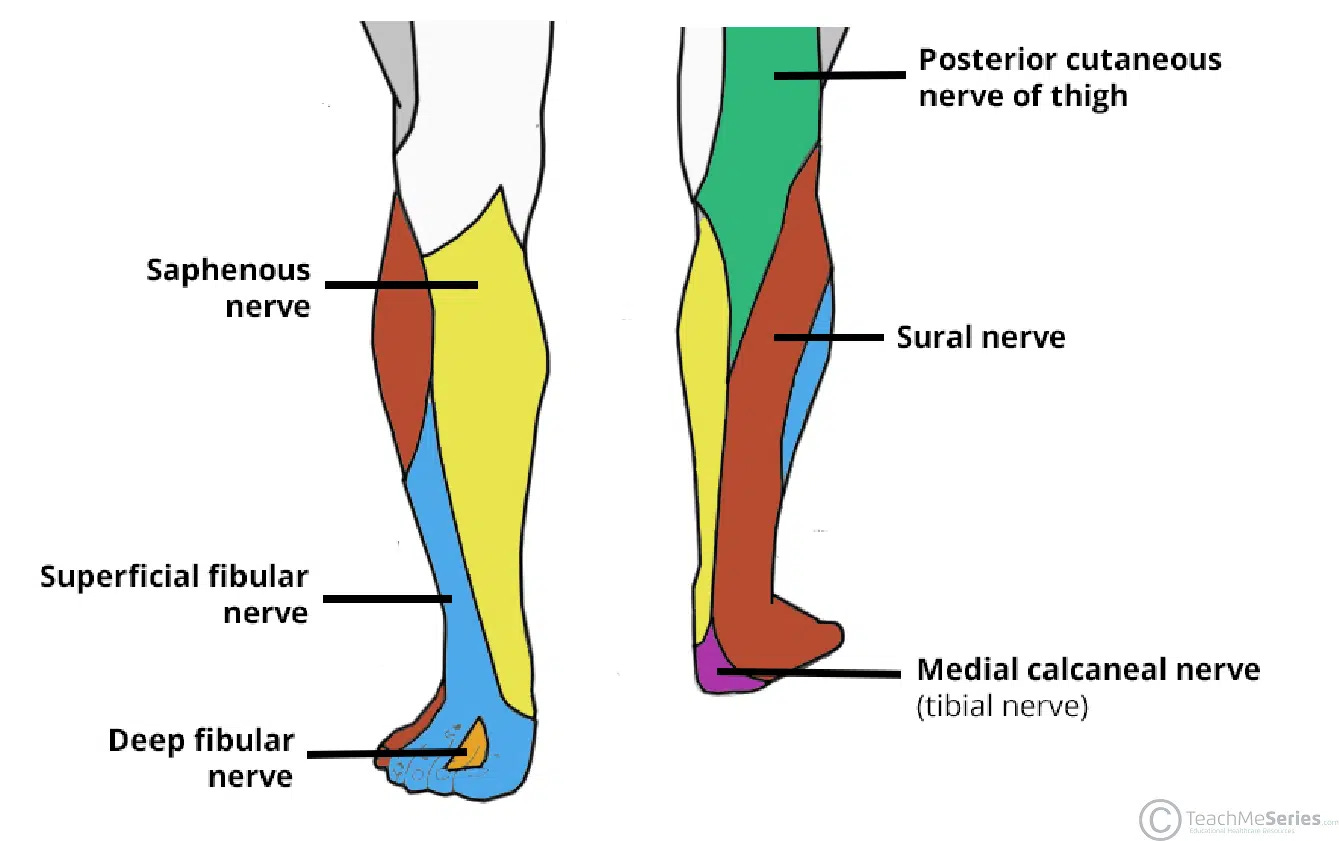
The potential suspects:
• Sural nerve: posterior (and slightly) lateral calf, Achilles, heel and foot
• Saphenous nerve: anterior-medial shin and medial calf and Achilles
• Posterior cutaneous nerve of thigh or tibial nerve1: posterior and upper calf area.
Why, exactly, those nerves are angry is where the real work begins.
Which brings us to…
Joe’s Sayings. Plumbing & Electric (for Effective Nerve Treatment). Because they are long, circuitous (and interconnected) structures, effective treatment tight and aggravated nerves takes a holistic approach.
To treat nerve pain, we have to act like a plumber or an electrician
For wrist or hand pain, parasthesias, or numbness, I add:
“An issue in the hand might be caused by a problem in arm, shoulder, neck or even head2.”
It is both astonishing and frustrating that much of our medical system fails to recognize the anatomical continuity of a single nerve extending from the head to the fingertip.
Far too many carpal tunnel releases are performed without even considering the nerve mobility and integrity from the lateral neck, through the thoracic outlet, for example.
To treat lower leg tension, we have to care about even more distance, as the sciatic nerve and its branches, also begins at the head and neck!
To treat any nerve pain or tension requires three areas of focus:
• Local: the immediate area of symptoms. For calf and Achilles pain, this would include examining the track of the specific nerve (e.g. sural) through the entire lower leg, ankle and/or foot.
• Regional: this involves the spinal level of the nerve root making up the nerve. The sural nerve is comprised of roots from L4, L5 and S1. Thus examining and treating the lumbosacral region is most relevant.
• Global: the entire spine, including head and neck (craniocervical). All nervous tissue originates in the head and neck. Thus for some cases, we must care about the integrity of this area.
Why This Affects Older Clients. Nerves and their fascia are more likely to get stiff and stuck with both age and activity. The more (repetitive, fascial-tensioning) activity — as seen in “old guy runners” with high mileage — the more likely there are tissue restrictions anywhere in the (local, regional, global) system!
Take-Away: if you’re older and highly-active, and you have stubborn lower leg pain, look beyond the calf muscle and Achilles tendon!
Joe’s Articles. A two-for this month:
• Work the Side Doors for Full Hip Mobility! Human, especially runners, are not “pieces of paper”, so it seems.
To unlock full hip mobility for runners often requires mobilizing lateral and medial hip, thigh and pelvic tissues.
For why, and how, check out (from iRunFar.com): Side-Door Strategies for Improving Hip Mobility.
• 3 Stride Strategies to Treat and Prevent Achilles Pain. Achilles tendon pain isn’t simply from running too much. There are three ways runners over-load the Achilles:
• over-stride landing (excessive energy absorption)
• excessive ankle plantarflexion push-off (calf and lower leg active over-use)
and:
• passive over-stretching in mid-stance: the “deflated” lower leg.
From iRunFar.com, Stride Strategies for Achilles Tendon Pain.
Over-striding is any time the foot lands (excessively) lands in front of the body. For Achilles overloading, this usually happens with a forefoot-loaded strike.
Excessive lower-leg push-off is more rare. Here’s an example:
Over-pushing with the lower leg looks…uncomfortable.
But “deflating?” It is both more common and often difficult to perceive…
Victory Friday. Inflating “Deflated” Lower Legs. This week I had two running clients present with a relatively uncommon, difficult-to-perceive, but very stubborn cause of pain in runners.
Client #1:
• New to running (< 3 year history)
• Chronic medial shin pain with low volume tolerance (pain with >30 miles per week)
• History of patellofemoral pain
Client #2:
• Former competitive high school and collegiate runner, recently returning to competitive — fast, track-based — training and racing
• Chronic lower bilateral lateral shin, ankle and foot pain
• History of bilateral lower leg stress fractures.
When I hear either of these stories, I assume I’m going to see lower leg strain. And that usually comes in the form of over-stride landing:
The primary sign of overstride landing is a vertical shin. Conversely, any time the shin is angled back toward the runner, that indicates landing energy will be absorbed: somewhere in the body.
However, in the video analysis of each client, I failed to see any significant over-striding.
Similarly, I failed to see awkward, straining signs typical of lower-leg over-pushing.
So I looked closer.
And what I saw, at mid-stance, is what I call a “Deflated Stride”.
A biomechanically-efficient leg at mid-stance should have only a slight amount of flexion at the knee and ankle, such that — at that moment, the knee should be at or behind a straight leg that runs from the chest to the toes:

A “Deflated” stride position occurs at mid-stance when the leg flexes excessively — at both the ankle and knee:

I call it deflated because it is like the two muscle groups in the leg responsible for maintaining upright — the quadriceps and the posterior lower leg (calf and shin) — are not fully firing, or at “full pressure”, at mid-stance.
This is a key descriptor because this lack of muscle strength is what causes tissue strain. When these groups — around the ankle, shin and knee — fail to maintain the stable (only-slighlty-flexed) joint position, they passively over-stretch: like blown shocks hitting a bump in the road.
Both clients were deflated. Both were passively straining lower leg tissues: Client #1 was over-stretch-straining both medial shins; #2, his lateral shins and ankles.
A clinical test of run-specific leg strength and stability is single-leg hopping, like this:
Runners should be able to:
• hop at least 3-4x per second (replicating a 180-240 step/minute cadence), and
• maintain only a slight ankle dorsiflexion and knee flexion — and not allowing that angle to change.
In other words, the client should be able to hop quickly with a stable, unmoving ankle and knee.
If not, this indicates a dynamic stability deficit consistent with “deflated running”!
Both clients were deficient: failing both in joint stability and “plyometric speed” and control.
Both were prescribed both concentric and eccentric lower leg and quad strength (examples: calf raises, single leg stepping) and single leg plyometric hopping drills.
Lastly, both were cues to run in ways to facilitate a stronger mid-stance position:
Client #1 was cued to run with a more vertical, hip-centric strategy — with a more powerful lift and fast-foot-to-ground strategy:
Client #2 was cued to use a pawback, foot-under-ground strategy: similar to the vertical but with a more rotary glute and hamstring utilization:
In the same visit, both runners demonstrated less “deflation” — better maintenance of relative knee and ankle extension — and with less perceived pain after both exercise and cueing.
Take-Aways.
• Look Out for (Mid-Stance) Passive Strain! Passive strain is a major tissue strain and pain generator, but it can be difficult to perceive in a runner’s stride.
• Assess & Prescribe Plyos! A good fail-safe is to always test for plyometrics strength with runners: if they fail the “speed and control test”, that alone is cause to prescribe plyo strength.
• Stride Optimize for Hips & Foot-Under-Body! But the most sustainable strategy to eliminate mid-stance passive strain is to optimize the stride: with a more hip-centric and foot-under-body running strategy!
Issue 87 is in the books! Do the world a favor: Please share this publication with people who want to learn more, and learn differently!
Thanks for reading, and have a great weekend,
The tibial nerve does not provide sensory innervation to the calf, but it may cause calf pain: it slides beneath the calf musculature at a junction called the soleal sling. Compression or tension there may cause pain, tissue restriction and a sensation mimicking a calf strain.
And, because of the neuro-fascial connectedness of the system, we often have to care about the lower spinal (thoracolumbar, pelvis) fascial system, as well. 😮💨