Victory Friday | Issue 120
Orthopedic Insights: Nerve Culprits for Common Leg Pains • Standing Closed-Chain Hip Rotary Power • Releasing (Half) the Drawbridge: the Importance of Comprehensive Fascial Treatment to Avoid Flare-Up
“The sage attends to the belly, and not to what he sees.” ~ Lao Tzu
Victory Friday is a weekly digest of reflections, insights, and tools from the world of functional manual and performance medicine. It is a free weekly publication. To support Victory Friday with a paid subscription, click below:
Happy Friday! A week of reminders: that hip impingement, inner knee pain and stubborn groin tightness…might all be tight (anterior) nerves, that loaded rotation is great for more athletic hips, and that fascial tension can create strange side-effects! Dive in and check it out!
What I’m Into: Nerve Culprits for Common Leg Pains. A few weeks back I took another Barral Institute neuromeningeal mobilization course for the leg nerves.
It served as a good reminder that some leg pain, stiffness, and dysfunction—which frequently present as orthopedic issues—are often actually driven by nerve tension or neural irritation.
Last week I shared some mobilization strategies for nerves of the front of the thigh1.
This week, properly placing the horse in front of the cart, I present some real-life examples of common orthopedic complaints and the anterior thigh nerves that may be causing that pain:
• hip impingement ➡️ femoral nerve or lateral femoral cutaneous nerve
• groin (or medial hamstring) strain ➡️ obturator nerve2
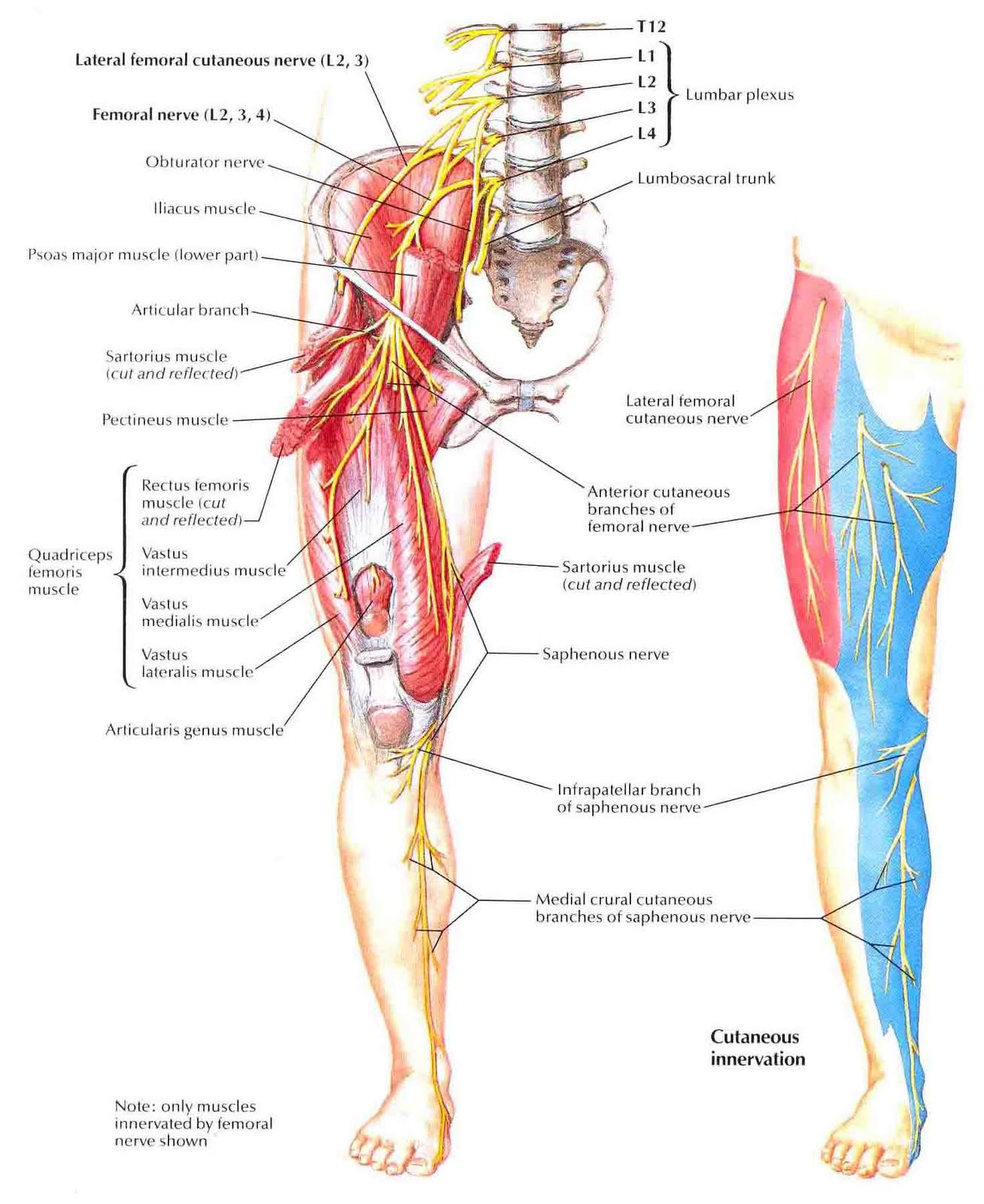
• medial knee and shin pain ➡️ saphenous nerve
• plantar fasciitis ➡️ tibial, medial plantar nerve
Takeaway: Don’t forget, nerves can hurt, too!
Cool Exercises I Like: Standing Closed-Chain Hip Rotary Power. Multi-directional hip and pelvic stability has been a major clinical focus this past year3.
For most, this includes beginning with the most basic, foundational hip stability and coordination work: on the ground4.
But most athletics — and life — occur on our feet.
From Ryan Lutke, CSCS (@fortifiedtraining) this staggered stance step-lunge exercise is a terrific progression:
What I like about it:
• weightbearing and dynamic, but only a moderate challenge: a tap-step (rather than a full-body step up)
• hip, pelvic and trunk rotational: emphasizing both the hip stability elements as well as the global pelvic and trunk stability system.
• strong, stable mobility: an exercise that can improve both strength and mobility simultaneously5.
• upper body loading challenges to trunk and legs. The med ball hold adds load into the rest of the body through the fascial system: a more robust (and specific) way to add hip resistance (compared to hip bands).
FotW & Victory Friday. Releasing (Half) the Drawbridge: the Importance of Comprehensive Fascial Treatment to Avoid Flare-Ups. It’s been a while since I’ve had a FotW6. This example isn’t a major error; however the following situation is a common issue with complex fascial work.
A few clients in the past month have presented with:
• stubborn pain, mobility loss, life limitations, and multi-system dysfunctions — issues in different physical systems, such as orthopedic and a GI/digestive issue
• a trauma history — usually impact trauma (falls, car accidents) and/or a surgery — often indicative of complex fascial tension
• the involvement of multiple body areas — a neck component and a limb, and a ribcage or abdominal dysfunction
A good example is my “speedy unicorn” from a few weeks back: a medial elbow pain with shoulder mobility loss…driven by fascial tension in the diaphragm and abdomen7:
• an orthopedic (functional) issue at the elbow
• a fascial tension problem from previous trauma (abdomen)
• findings locally (elbow stiffness), regionally (mobility and efficiency loss at the shoulder complex) and globally (fascial tension in the ribcage, diaphragm and abdomen).
That was a great case because we quickly identified the true driver (abdominal fascia) and got immediate and sustained relief from treating the fascial restrictions — without any side effects or complications.
But not all cases are that simple.
This past month I’ve had a few similar cases where:
• I perform a fascial treatment to key areas (guided by subjective and objective findings, as well as Barral Institute General Listening Techniques).
Then:
The target area feels better, but side effects — often very strange ones — occur.
Examples include:
Two clients with abdominal pain/tightness (one two months ago, one last month) with acute lower leg pain and tension (one was ankle pain, the other, “really tight calves”) following a diaphragm treatment.
One client — primary complaint of abdominal pain and bloating — had a flare in several body areas: left anterior thigh and left medial knee8, and left lumbar-pelvis, following a left-sided diaphragm and visceral (stomach and small intestine) treatment.
In both cases:
• I did a potent fascial input (specifically: to the diaphragm)
• the client had “random” flares in other body areas
and, as it turned out:
Both had lingering fascial tension elsewhere in the system,
which became more prominent after the releasing treatment
The best analogy I can come up with:
• a complex system is under tension from multiple areas — like a drawbridge
• significantly releasing some tension is crucial — but if you only release one area (or, not enough in all relevant areas) — there is an increased tension gradient that can be more problematic than the original issue!
It’s like lowering a vertical drawbridge…but only on one side:
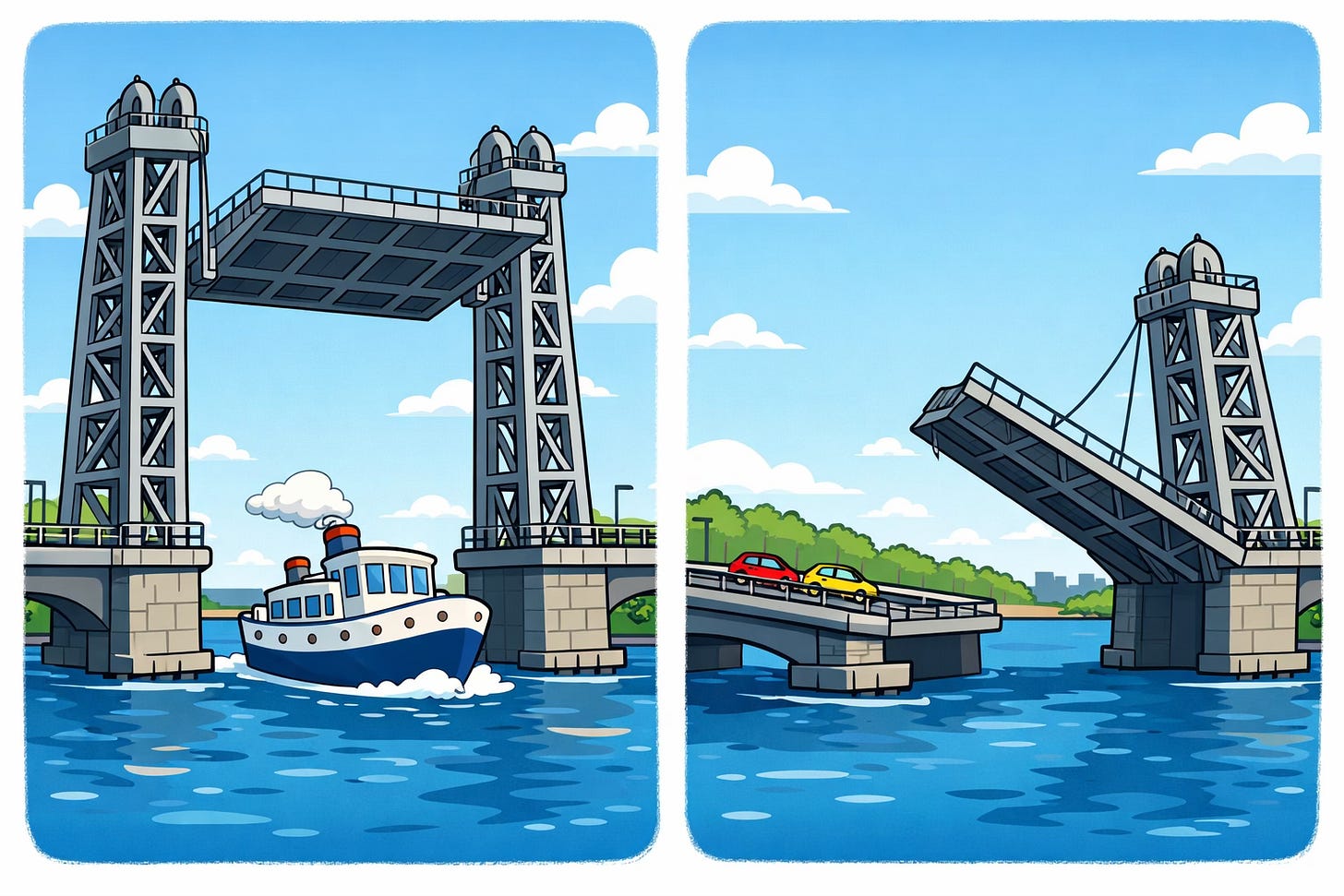
For Example #2: this client had significant restrictions in the left diaphragm, stomach and small intestine. Thorough treatment was performed there.
But after she returned, reporting the left-sided flare-up, repeat examination showed profound right-sided diaphragm tension (that was not detected the previous visit).
The theory:
• there was significant fascial tension around the upper abdomen and diaphragm on both sides (likely: left slightly more than right)
• releasing predominantly the left side only created a tensional imbalance: the right diaphragm tension effectively placed a dysfunctional pull on her entire left side: left abdomen, pelvis, hip and lumbar plexus — which would account for all over symptoms.
• untreated downstream tensions — particularly in lower legs — can contribute to such imbalances (this client also has a chronic ankle sprain history).
Consequences. Neither flare-up was major, but certainly inconvenient and tedious. But it was a good lesson to evaluate the entire fascial system
Takeaways. Evaluate the Whole System & Have a Fascial Mobility Plan! A more thorough mobility assessment may have helped catch the subtle-but-signficiant tensions I missed.
However, sometimes the better bet is to arm your clients with a holistic fascial mobility plan:
• subsequent to the left-sided flare, I taught my client both visceral mobilization with. ball:
and I showed her a specific technique for using a tennis ball on the margin of the anterior diaphragm: a key area of tension for her.
Because fascial tension — and rebalancing after a mobilization — can be unpredictable, often the best bet is empowering clients to “right the bridge”, themselves!
Issue 120 is complete!
Help people move, function and feel better: please share this publication!
Thanks for reading, and have a great weekend,
Issue 119: Targeted Front-of-the Thigh Nerve Glides. Taylor Kruse (@kruseelite) provides targeted nerve glides: femoral nerve (straight-leg anterior tension with spinal flexion/extension), obturator nerve (hip abduction emphasis), and lateral femoral cutaneous nerve (hip adduction with trunk side-bending).
Perform these gently at 3/10 intensity, as nerves glide rather than stretch and are highly sensitive when irritated.
Issue 75: Obturator Obfuscation. A client with a complex high hamstring tear history, multiple surgeries, and two years of crutch dependence showed slow, fluctuating progress with a comprehensive treatment plan. Lingering medial hamstring pain and tightness —worse with hip abduction/opening while sitting — revealing strong positive obturator nerve tension (seated slump/abduction test), indicating obturator involvement mimicking sciatic/hamstring symptoms. Targeted upper/medial thigh fascial mobilization with dynamic adduction/internal rotation to slacken the obturator nerve yielded lasting improvement without flares, emphasizing the need to assess less common nerves like the obturator in stubborn proximal leg pain.
Issue 84: Signs of (Severe) Sacroiliac Joint Sprains, and Subtle Subclinical Sacroiliac Strains. The signs of classic (severe) SI joint instability and more subtle, subclinical but functionally significant SI joint dysfunction.
Issue 89: “Belt it Out!”: Functional Sacroiliac Joint Instability Diagnosis & Treatment Using a Belt. Signs and symptoms of sub-clinical sacroiliac joint instability — including mobility loss, weakness and motor control deficits — and how pelvic stabilization can improve these otherwise longstanding and stubborn deficits.
Issue 105: Joe’s (Hip) Six-Pack. A three-dimensionally strong hip will enhance not only focal strength and stability but also hip and leg mobility and overall athletic efficiency. This six-pack of exercises enhances coordination and stability in all six movements of the hip joint. Strength exercises include: prone hip internal rotation, sideplank clamshell external rotation, sidelying adduction, sideplank abduction, banded supine hip flexion and double- and single-leg bridging.
Issue 19: The Mobility-Strength Continuum is the idea that all movement lies in a continuum between purely passive (full range, minimal contractile) motion, and pure strength (mid-range, maximal load and muscle contraction). Touching all aspects of the mobility-strength range is key for optimal health. But combined, nearly-full motion and active strength may be the most functional.
“Flounder”, or perhaps a different “F”.
Issue 116: Speedy Unicorn: Zero-to-Weird Success in Three Visits. A 60+ client with persistent left medial elbow pain saw no lasting relief from initial orthopedic treatments (soft tissue/joint mobilizations, stretching) or subsequent craniocervical/neurogenic approaches. Only after identifying major abdominal surgical scars (childhood kidney surgery and recent rectal prolapse repair) and treating layered visceral/abdominal fascial restrictions with upper extremity motion did she gain immediate, significant elbow pain relief (gone for days) and better neck mobility. The case underscores the power of quickly abandoning partial results to systematically uncover rare distant causes like visceral-fascial connections instead of persisting with local care.
See “What I’m Into” and anterior hip and thigh nerves.





Love the drawbridge analogy for fascial tension imbalances. The example of releasing one side creating increased tension gradients elsewhere makes perfect sense when you think about interconnected systems. I've had similar experiences where treating one area produced unexpectd symptoms downstream, and it took a while to realize the whole system needed rebalancing. The emphasis on arming clients with self-mobilization tools is pratical and empowering.