Victory Friday | Issue 88
Orthopedic Insights: Point to the Pain • Pronate More for Achilles Relief (& Joe’s Heel Bone Self-Mob) • Deepening the Groove at Western States • Obturator Internus and the “Internal” Pelvis
“Live the questions now. Perhaps you will then gradually, without noticing it, live along some distant day into the answer" ~ Rainer Rilke
Victory Friday is a weekly digest of reflections, insights, and tools from the world of functional manual and performance medicine. It is a free weekly publication. To support Victory Friday with a paid subscription, see below.
Friday’s here! Stuck with stubborn pelvic (“hamstring, butt…I dunno!”) pain? Achilles still hurt (even after treating the nerve? Some hard-earned nuggets on both, this week!
What I’m Into: Point to the Pain. When a person has pain, it’s crucial they — as best as possible — point to the exact location of their pain.
(Then, ask an additional question: “When you push on it, can you feel [replicate] your pain?”1)
Then, if possible, the clinician must get their hand(s) on that exact point.
Why? It rules in — or rules out — specific structures.
Too often a client will vaguely indicate — waving a hand at — a pain area, then apply their own descriptor.
Example 1: A client, while seated, facing you, rubs on their lower spine and pelvis saying, “I have back pain.”
But where and what, exactly, hurts? Thoracolumbar? Lumbar? Lumbopelvic? Lumbosacral? Sacroilliac? Sacro-coccygeal? Cervicothoracic??2
All of these structural zones — each with a distinct bony-joint-tissue type and biomechanical function — could generate pain and have both widely varied causes and treatment strategies.
Example 2: Two clients this week presented with posterior hip-and-pelvis pain.
One described it as: “hamstring pain”.
The other, “hip and butt pain”.
For both, it was the obturator internus muscle (see Victory below).
Cool Exercises I Like. Pronate More for Achilles Relief (& Joe’s Heel Bone Self-Mob). Last week I wrote about one oft-overlooked factor in chronic Achilles and calf pain3.
This week, the folks at The Manual Shop posted this gem of a treatment progression for a common — but completely overlooked — cause of chronic Achilles tendinopathy:
A stiff, inverted4, calcaneus.
You see, most tissues in the body are meant to be loaded in a very specific way.
Long bones take enormous weight with straight vertical compression; but take very little force (before breaking) at angles5.
The same is true for the Achilles. It is meant to take enormous impact loads — then store that energy (for a split-second) then rebound it to create propulsion.
And the Achilles is meant to be loaded in straight-vertical orientation.
But what if it becomes angled?
Antonio Colletti, PT walks us through a case of bilateral Achilles pain, driven largely by heel bones stuck in too much inversion:

The heel bone is inverted, but holistically: the foot is stuck in excessive rearfoot supination.
This is where one begins the stance gait cycle: land on the outer foot (in supination), then gently rolling medially — into pronation — until reaching the medial arch, ball of the foot and big toe.
But if the foot is stuck in supination?
A heel bone that can’t evert6 will load the Achilles — from midstance to push-off — at an angle, causing inefficient strain.
And:
A foot complex that can’t achieve medial foot and big toe loading will lack efficient, athletic hip extension push-off.
Here’s The Manual Shop showing us how to correct that calcaneus and restore efficient foot and ankle motion:
But the key move? Something I call, “The Anti-Orthotic”:

It’s the anti-orthotic because it is the opposite position and movement that most conventional orthotics promote.
Some people need medial arch support — especially those with hyper-mobile, “collapsed” mid-foot structures.
Many more people, however, are over-prescribed orthotics that over-correct into excess supination, never allowing the foot to “finish” into moderate pronation.
Joe’s Calcaneal Eversion Self-Mob. If you have chronic Achilles tendon or any pain in the heel area — and your heel bones look like those pictured above, you can try this self-mobilization strategy:

Simply:
• Be seated, crossing the stiff foto and ankle on the opposite knee.
• For a left heel: stabilize the left lower leg by grasping just above the ankle.
• The right hand will grasp the heel bone and try to:
A. distract the heel bone inferiorly (diagonal arrow)
B. laterally glide the heel bone (vertical, downward arrow)
Push on and off repetitively. The motion may be minimal (this is hard work) but even a few millimeters can help restore efficient motion and improve the alignment — and loading character — of the Achilles!
Give it a try!
But if you can’t, find a physio with good hands-on skills and a Systems-based treatment approach7 to help you overcome chronic Achilles pain!
Joe’s Articles. Deepening the Groove at Western States. This is non-sports medicine content, but some insightful tips for my favorite race — and all hundred-mile trail runs!
From iRunFar.com, The Western States Killing Machine, Part Three: Deepening the Groove.
With fun stories and insights from Billy Yang, Didrik Hermansen, and Tyler Green, here are new tips gleaned over the past decade of Western States Endurance Runs:
Pacing: Balanced pacing is key to avoid Western States 100 pitfalls. Overly cautious pacing disrupts biomechanics, causing fatigue and stiffness. Runners should maintain a sustainable, fluid "all-day" effort honed in training to work with the course and maximize performance.
Nutrition: Disciplined fueling is crucial for sustaining energy over 100 miles. "Hyper-preparedness" implies nutrition supports pacing and handles course demands like climbs and heat, preventing energy depletion and physical breakdown.
Using Downhills as a Gift: Leverage the 22,970 feet of descent as an opportunity. Train for efficient downhill running to preserve quads, using a relaxed stride to minimize fatigue and boost momentum on runnable sections.
Victory Friday. Obturator Internus and the “Inverted” Pelvis. Had a couple remarkable breakthroughs with two clients with posterior upper thigh/hip and lower pelvis pain.
Per above:
One described it as: “hamstring pain”.
The other, “hip and butt pain”.
But when I asked them to “Point to the Pain” — and when they confirmed it with my own palpation — we landed on the medial side of the ischial tuberosity of the pelvis.
On the inside of the obturator foramen.
On the obturator internus muscle:
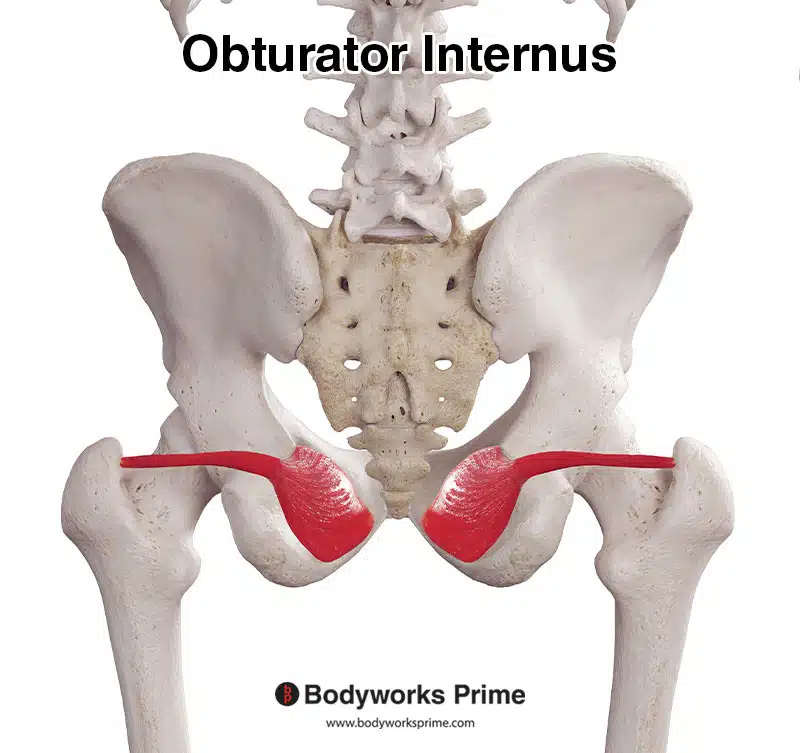
The obturator internus is a small hip stabilizer muscles, known as one of the “Deep Six” hip external rotators:
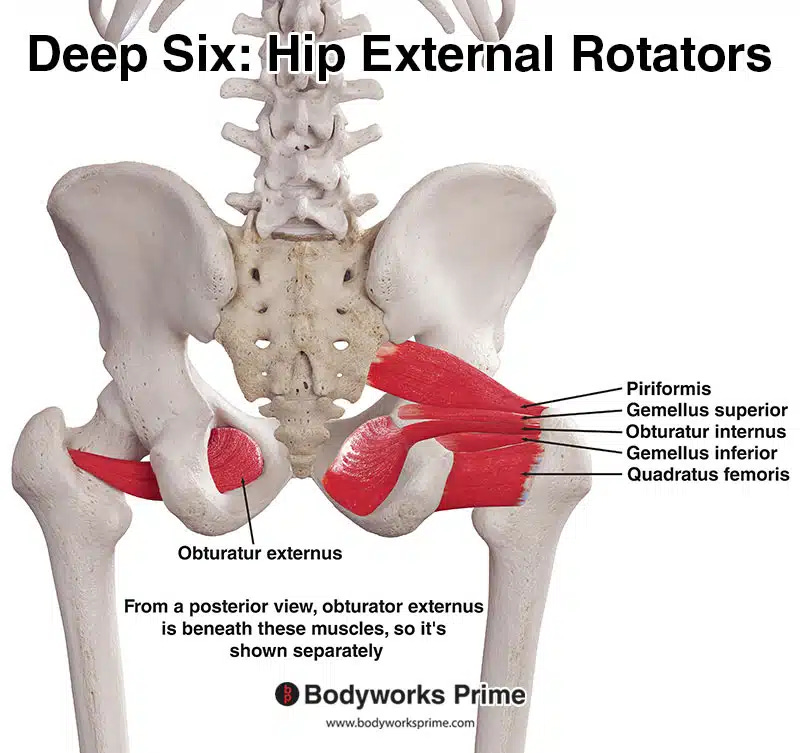
While their motion function is external rotation, the Deep Six are, at their core, the deepest hip stabilizers: crucial for both stance stability and a strong, coordinated push-off with both walking and running.
Palpating, then massaging, stretching and resisting motion of that muscle (Cyriax Myofascial Testing8) were all painful.
What & Why: The Role of the (Dysfunctional) Pelvis. It’s one thing to massage, stretch and strengthen the obturator internus.
But why is it tight, weak and painful?
With both clients: the painful side pelvis was stuck in adduction — and limited in abduction.
In other words, the pelvis was shifted9 medially. Like the calcaneus in the story above, it was inward angled (from top to bottom). This inverted/adducted angle was putting excessive strain on this little — but crucial — hip stabilizer.
Additionally — for one of the clients — the opposite hemi-pelvis was lacking in the opposite motion:
• the left (painful side) pelvis was stuck “in”
• the right (opposite) pelvis was stuck “out”
Like two windshield wiper blades, both sit bones were angled to the left!
Restore Pelvic Motion & Alignment. Thus, apart from direct treatment to their painful area (both crucial for recovery and for validation10 ), I endeavored to restore full and equal pelvic opening (abduction) and closing (adduction).
Stretching into pelvic abduction/opening:
And pelvic adduction/closing:

Push/Pull Both Ends! I performed pelvic abduction mobilizations with specific force on both ends of the pelvis: at the iliac crest and (“delicately”) the ischial tuberosity. This more focused approach at the ischium is often necessary to correct a stiff, inefficient lower pelvis.
Then I reinforced with a home program for pelvic opening and closing, per the exercises above.
Stretch and Strengthen the Obturator. Finally, I dusted off a couple specific obturator internus exercises. I will share these next week.
Take-Aways. A few keys for this one:
Point to & Touch the Pain! Find the exact structure, if possible. Don’t rely on general descriptors (and especially, the anatomical descriptors of clients). For neither one was their pain “hamstring” or “hip” (joint) or “buttocks” (gluteal muscles).
Specificity led us to the true structure.Treat the Joint Around The Muscle. A dysfunctional muscle needs both bony ends — and the opposite side — efficient! Simply massaging, stretching and strengthening the obturator is insufficient for sustained resolution.
Evaluate and treat the efficient movement of the muscle bookends: the pelvis and the femur.
And don’t forget the opposite side: pelvic dysfunctions are often paired, and a dysfunctional right side may stress the left!
Issue 88 is complete!
People need real, usable information that challenges a lot of (useless) orthopedic paradigms.
Know folks who might need new ideas and a fresh approach to pain relief, function and wellness? Please share this publication!
Thanks for reading, and have a great weekend,
This is a key structural (local) versus referred pain diagnostic. If they know where the pain is — but can never truly “touch it” — it is likely referred from elsewhere.
Sometimes, a client will present with “back pain” that is even lower neck-upper ribcage (as, to some clients, anything on the “back” of the spine is considered back pain).
Issue 87: “If You’re Over 40, It Might Not (Actually) Be Your Calf or Achilles”. A post on differential diagnosis for chronic calf and Achilles pain: namely, nerve tension and nerve pain in the lower leg, ankle and foot.
“Calcaneal inversion is the inward tilting or medial rotation [from top to bottom] of the calcaneus (heel bone) relative to the tibia, where the sole of the foot faces inward.” ~ Grok
Issue 4. Load versus Efficiency: The Soda Can Test. To demonstrate tissue specificity, I take an empty soda can. Smashing it straight into the ground, it can withstand significant force before deforming. But angle it just slightly? The cylindrical structure dents at a fraction of the impact. Most body tissues function with similar specificity.
“Calcaneal eversion is the outward tilting or lateral rotation [from top to bottom] of the heel bone (calcaneus) in the frontal plane, turning the sole of the foot away from the body's midline.” ~ Grok
Issue 41: Systems & Dimensions. Full and sustained pain relief and recovery of function often requires a comprehensive treatment approach of multiple Systems (body areas: spine, pelvis, abdomen, pelvis, hip, knee, etc) and Dimensions (types of tissue: muscle, tendon, bone/joint, fascia, nerves, blood vessels, etc)
A definitive test to rule-in a specific muscle group as painful or strained is if it is: painful at palpation, painful with passive stretch, and painful with resisted action.
In this case, the obturator internus was tender to palpation, sore to stretch (into passive hip internal rotation), and sore with resisted hip external rotation.
or bent, or torsioned, or warped, depending on your perspective of pelvic motion.
As one of the clients reiterated — “so you would believe that I wasn’t making it up!”






