Victory Friday | Issue 122
Orthopedic Insights: “I Already Did That! (But Not Enough)” • Rotational Hamstring Rehab • Hip Rotational Efficiency, Part 1 • Chicken or Egg? Eat ‘Em Both: Ending 40 Years of Running Knee Pain.
“Sow a thought, reap an action; sow an action, reap a habit; sow a habit, reap a character; sow a character, reap a destiny.” ~ Lao Tzu
Victory Friday is a weekly digest of reflections, insights, and tools from the world of functional manual and performance medicine. It is a free weekly publication. To support Victory Friday with a paid subscription, click below:
It’s another Friday! Big running wins this week, including stronger (more rotational) hips, happier (less rotational) knees, and a commitment to persistence and patience. Let’s dig in!
Joe’s Sayings. “I Already Did That! (But Not Enough)”. A highlight of my fellowship year with the Institute of Physical Art was the twice-weekly mentored treatment sessions. As Fellows-in-training, we treated real clients while mentors joined us—stepping in for a few minutes at the start and end of each session, observing throughout, and offering insights and recommendations to optimize the treatment.
They were profoundly helpful — the privilege of having another set of hands, eyes and a expert brain — providing insight to a real case, a real person, in front of you.
But such sessions sometimes required a thick skin and humility, as the mentor would frequently point out corrections, or outright omissions, to your treatment strategy.
It was easy to get defensive. But if you could check your ego at the door, both the client — and your clinical skills — got vastly better.
I was pretty good at that. I wasn’t the smartest, but I was eager to learn and could take all types of feedback.
Some were less good.
A favorite story I heard oft-repeated from IPA Founder and ultimate mentor, Gregg Johnson:
• He would enter a room for mentorship and find key dysfunctions he felt required treatment
• When stating his recommendation, the fellow-in-training often replied, “I already did that!”
Then, he’d make a face that looked something resembling:
👀😳😑
From that story — and the lived experience of having to re-do what I have already done, comes this quote I often use — for myself and my clients — today:
“Just because it’s been done before doesn’t mean it’s been done enough!”
In theory, a specific treatment — such as the mobilization of a stiff thoracic vertebra or ankle joint, a myofascial technique, a core muscle facilitation, or even a posture or motor control cue — should be “one-and-done”: do it once, and it gets — and stays — better.
But that isn’t always the case.
Yet when executing a plan of care, once a technique has been done we often cross it off the list. Yet when a client fails to recover as quickly and fully as desired, we fail to reconsider that already crossed-off item.
That is when a second pair of eyes and hands is so crucial. They are unaware and unfazed by what has been done. Simply, they ask:
Does it need to be done (again), or not?
Areas with high stubbornness, intertwined with other dysfunctions, or resulting from repetitive stress often need much higher frequency and high volume treatment.
Common dysfunctions requiring repeated manual treatments:
• post-traumatic tissue adhesions (impacts, cuts, surgeries)1
• visceral restrictions2
• fibular dysfunctions3
• any deep, dense fascial restrictions
So anytime I return, yet again, to a stubborn area, I find myself saying that — to reassure both myself and my client:
It’s enough when it’s gone and stays gone. Until then? Keep at it
Cool Exercises I Like. Rotational Hamstring Rehab. I like to say that true athleticism — and most dysfunctions live in, and injuries are borne from — the transverse plane: the top-down rotations that occur from head to toe.
The folks at David Grey Rehab (@davidgreyrehab) recently posted a terrific series to enhance hamstring injury rehabilitation using transverse rotation movement and loading:
Why I Think This Works. There are two reasons that transverse plane rotation is so helpful, in particular, for hamstring injury recovery:
Athletic movement, and whole-body fascial patterns, are rotational (and not just sagittal. As they state in the post, ineffective rehabilitation often consists only of sagittal plane exercises: “Nordic curls, RDL’s, and glute bridges: all with zero rotation”.
Rotation loads the hip (to do its share of work). If you observe closely, three of the four demonstrated exercises involve potent hip internal rotation (which, among other things, accesses “The PILC”4 to achieve full glute muscle engagement).
And I’m convinced most chronic hamstring injuries are caused by glute under-functioning.
Joe’s Articles. Hip Rotational Efficiency, Part 1. I shared a Victory Friday recently highlighting the major running performance improvements from optimizing ball-in-socket rotation efficiency5.
This “on-axis” mobilization and coordination approach has now graced the pages of iRunFar:
Understanding and Improving Hip Efficiency, Part 1
TL;DR:
Intro: explains hip efficiency for runners, why hips often stay stiff/weak despite both stretching and general strength, and starts with mobilization before reinforcing with coordination strength (part 2).
Hip Efficiency: Smooth, low-resistance ball-and-socket motion powered by coordinated ~21 hip muscles; keeps femoral head centered for powerful, efficient stride.
Common Issues: Persistent stiffness, strength plateaus, chronic problems, reduced performance — often from inefficiency and poor coordination.
Core Problem (Tug-of-War): Mis-coordinated muscles pull femoral head off-axis (forward glide on IR, backward on ER), causing friction, stiffness, overcompensation, and inefficiency cycle.
Fix Foundation — Release & Realign: Myofascial release to free tissue and restore proper alignment/translations; daily foam rolling reduces density and asymmetry.
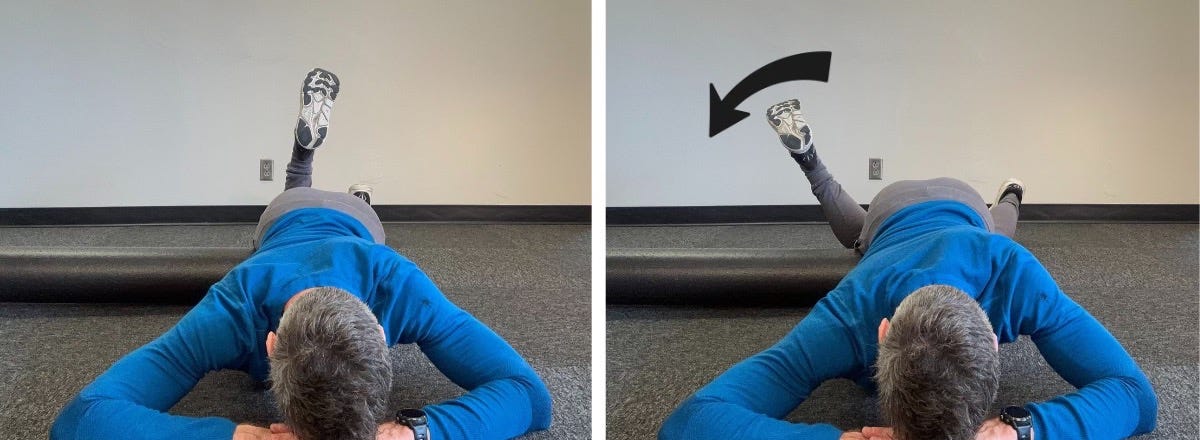
Anterior Mobilization: Tissue release with prone roll on anterior/lateral hip (2–3 min/side):
On-axis mobilization: bent knee internal rotation oscillation with anterior hip on roll (3 × 30 sec daily):
Posterior Mobilization: Tissue release with crossed-leg glute roll (feel “baseball in pillow”), pelvis rotated 30–45°.
On-axis mobilization: Add crossed-leg oscillatory external rotation with posterior hip on top of roll (3–5 min/side daily):Next Step: Continue daily until symmetry improves, then pair with resisted rotation strength (Part 2)
Victory Friday. Chicken or Egg? Eat ‘Em Both: Ending 40 Years of Running Knee Pain. I saw as a new client a few weeks ago a 60 year old, athletic man, with a 40-year knee pain history.
Thankfully, he wasn’t stubborn: he’s had some sort of running-induced knee pain dating back to post-high school: attempts to run more than a few miles resulted in knee pain: both at the end of runs, and soreness/stiffness lasting into the next day.
If he tried to run consecutive days, it would hurt more.
So, by and large, he didn’t.
For nearly 40 years.
While he tried various strategies — including several bouts of physical therapy — over the years — nothing fully abolished his pain.
He recently had yet another orthopedist consult. Imaging revealed no serious pathology: no arthritis, no soft tissue abnormality. Great news6.
On the recommendations of both friends and coworkers, he sought me out.
Impressively (if not outlandishly), he has a new goal: completing a 50-kilometer trail race.
Over the course of three visits, we identified two crucial dysfunctions that — now in correction — have significantly reduced his knee pain and will soon eliminate it.
Knee torsion. His painful knee was excessively rotating in a complex way: his tibia would externally rotate as his knee flexed (as in lowering down a step); his femur would internally rotate, then — at about 20 degrees flexion — would rapidly externally rotate.
This created a “whip”-like movement, as the knee complex would appear to valgus, then rapidly translate (shear) laterally.Running inefficiency. On visit three, when we finally watched him run, we saw two significant inefficiencies:
• his cadence was profoundly low: between 130 and 140 steps per minute! He spent way too much time on the ground, with his legs absorbing excessive impact energy
• his painful knee was performing the same “whip” in initial contact to mid-stance: a mild valgus then a rapid lateral shear.
I was stoked.
“That’s your pain!”
Treatment Approach. We performed the following:
• Torsion correction to the knee. As the knee is half the hip and half the ankle, we optimized alignment and mobility of the ankle below, the hip, pelvis and ribcage above, and the knee with targeted manual therapy and hip mobility and strength.
then, once we identified the cadence and knee stability deficits:
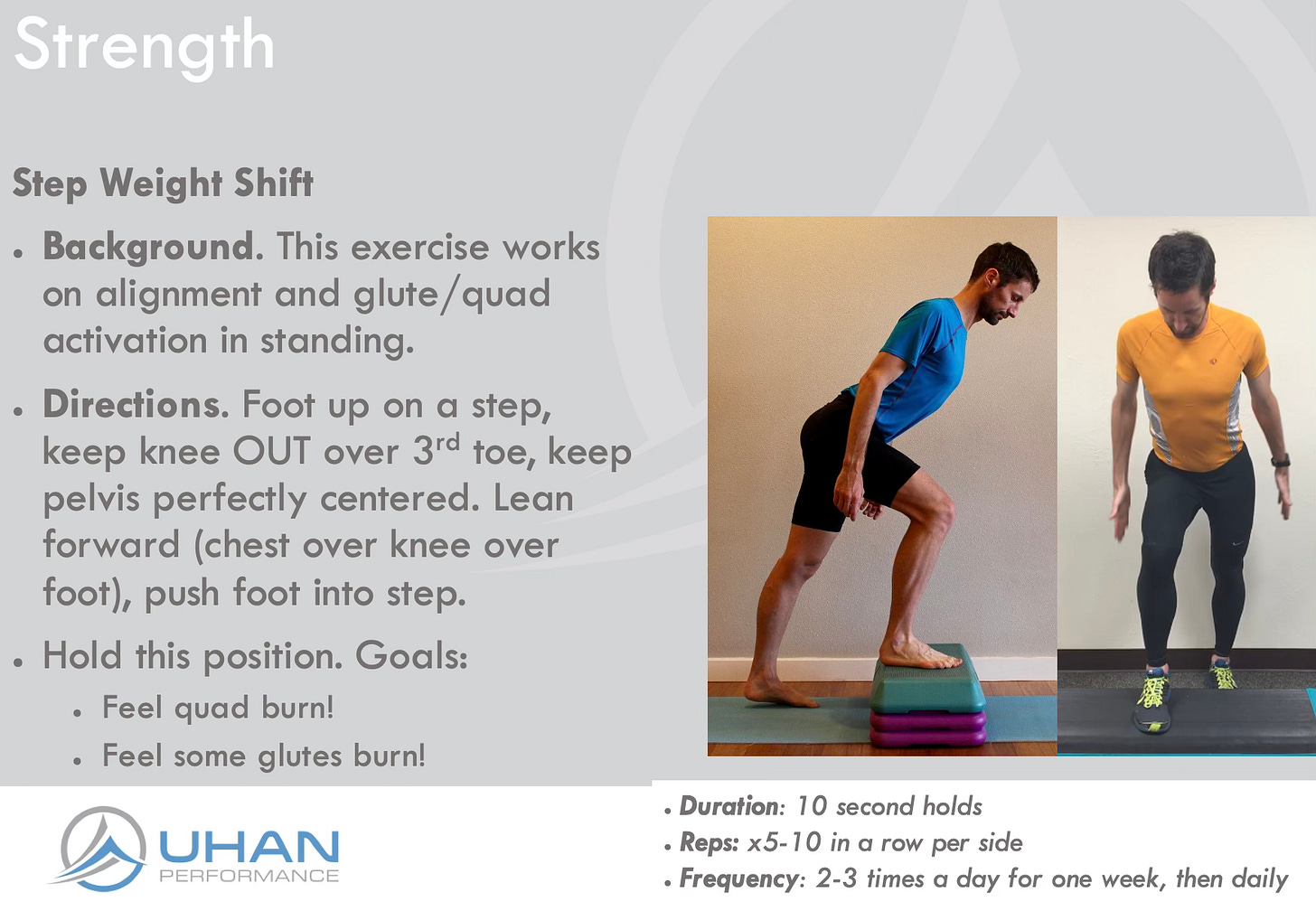
• Neuromuscular stabilization for the knee. We shored up his knee stability, first with the quad, from above. This includes isometric holds in the mid-stance running position (the “Step Weight Shift” courtesy of my great mentor, Jeff Giulietti).
He was doing a lot of single leg quad exercise in the gym but couldn’t “feel his quad” until he did these prolonged holds:
• Stabilization for the lower leg. To ensure his lower leg could also stabilize, we performed single leg heel raises (with which he was weaker on the left), then a light hopping series — double and single-leg hops with emphasis on a slightly-flexed but stable knee and ankle.
Then, specific to stride optimization:
• Increased cadence via increasing arm swing rate. For this client, a faster arm swing was the easiest and most sustainable way to improve foot-to-ground stride rate.
Similar to a previous Victory7, this one pleased me — both for its complexity (finding and resolving a multi-decade problem) and its speed.
He is currently ramping up his running volume and frequency with not only less pain but a faster pace and more strength and comfort!
Big wins en route to his first ultra!
Take-Aways. You Gotta Watch ‘Em Run…and Optimize It. The interesting question for this client is:
What came first? The ultra-slow cadence, energy-absorbing stride — which created the knee instability? Or the torsioned, inefficient, unstable knee that made a quick cadence, efficient running stride an impossibility?
Ultimately, it doesn’t matter. We needed to optimize both.
His most recent PT before me was a “running specialist”, yet even they failed to adequately observe his knee dynamics, or attempt to optimize his running form.
Without addressing the stride, it’s unlikely the mobility, alignment or strength treatments would sustainably relieve the pain. The run stride had to be optimized to limit the excessive knee load.
Watch ‘em run, and don’t be afraid to optimize!
Issue 122 is complete!
Help people move, function and feel better: please share this publication!
Thanks for reading, and have a great weekend,
as my friend, colleague and fascial expert Garrett Petry says, “Energy In, Energy Out.” If a body area absorbed high energy, it often takes high energy — time, intensity, volume — to fully restore.
especially if due to recurrent stressors (GI dysfunction; endometriosis)
Issue 121: More Fantastic Fibula Wins! Mobilizing fibular dysfunctions may be a key driver of rapid, systemic improvements in lower-limb function. Mobilizing the fibula (along with surrounding fascia, compartments, syndesmosis, and nerve branches) restored ankle dorsiflexion in chronic stiffness, dramatically increased knee flexion (+15°) in a pre-knee-replacement client with valgus deformity (without direct knee work), and quickly reduced lateral hip/knee/calf tightness and improved walking tolerance in a chronic hamstring/sciatica case. These outcomes underscore the fibula’s dynamic role and strong fascial influence, making lateral shin/fibula work a high-yield target for lower-body mobility and pain relief.
Issue 2: The Posterior-Inferior-Lateral Corner of the hip. The back-outer aspect of the hip joint is key area to access for both maximal efficiency and strength (via optimal gluteal stretch-activation). When this area is too tight, the hip cannot move enough, nor can it stretch the gluteals sufficiently to produce peak force.
Issue 118: 3D Hip Efficiency Performance Win! A runner-mountaineer client with stubborn hip stiffness showed immediate performance improvement after “on-axis” hip treatment: targeted foam rolling (anterior for right hip, posterior for left) plus hands-on mobilizations with rotation and traction. Retesting revealed better femoral alignment, improved hip mobility, and a striking performance boost—15–25 seconds faster per mile during that day’s run (from ~7:00 to sub-6:45 pace).
Interestingly: for many people, this is bad news: they want an answer, even if it is a terminal one (surgery, knee replacement). For me, the absence of serious tissue damage simply means a mechanical dysfunction is present — one that causes pain, but hasn’t caused damage. Yet.
Issue 116: Speedy Unicorn: Zero-to-Weird Success in Three Visits. A 60+ client with persistent left medial elbow pain saw no lasting relief from initial orthopedic treatments (soft tissue/joint mobilizations, stretching) or subsequent neck/nerve approaches. Only after identifying and treating major abdominal surgical adhesions (with paired upper extremity motion) did she gain immediate, significant elbow pain relief, as well as better neck mobility. The case underscores the power of quickly abandoning marginal results to systematically uncover rare distant causes like visceral-fascial connections instead of persisting with “logical” care.